Over the last several years, celebrating our melanin and the magic we possess has garnered both attention and admiration. For some, like Winnie Harlow and the legendary Michael Jackson, vitiligo caused them to learn to embrace the skin they are in. Their bold and empowering presence has shattered societal norms and created a deeper understanding of vitiligo.
Around 1% of the US population has some form of vitiligo, but nearly 40% is believed to be undiagnosed.1 Vitiligo affects people of all ages, gender, and ethnicity equally. But, in the black community, it challenges the beauty standards that emphasize smooth, even skin tones.2 Shedding light on vitiligo helps to promote understanding and acceptance of this condition.
What is Vitiligo?
Vitiligo is a long-term skin condition for which there’s no cure. The loss of melanocytes, the pigment-producing cells in the skin, characterizes it. This loss results in white or lighter patches (depigmentation [dee·pig·muhn·tay·shn]) appearing anywhere on the body.
There are several different types of vitiligo. Which kind you have depends on its location, distribution, and progression. Some of the common types of vitiligo include3-6:
- Generalized or non-segmental vitiligo: This is the most common type of vitiligo, where depigmentation occurs on different parts of the body.
- Segmental vitiligo: This type of vitiligo affects only one side or a segment of the body.
- Focal vitiligo: In this type, small patches of depigmentation occur on small areas of the skin.
- Mucosal vitiligo: This type of vitiligo affects the mucous membranes, such as the lips and the inside of the mouth.
- Universal vitiligo: This is a rare type of vitiligo where almost the entire body is affected.
- Acrofacial vitiligo: This type of vitiligo affects the face, hands, and feet.
- Mixed vitiligo: This type combines two or more of the above types.
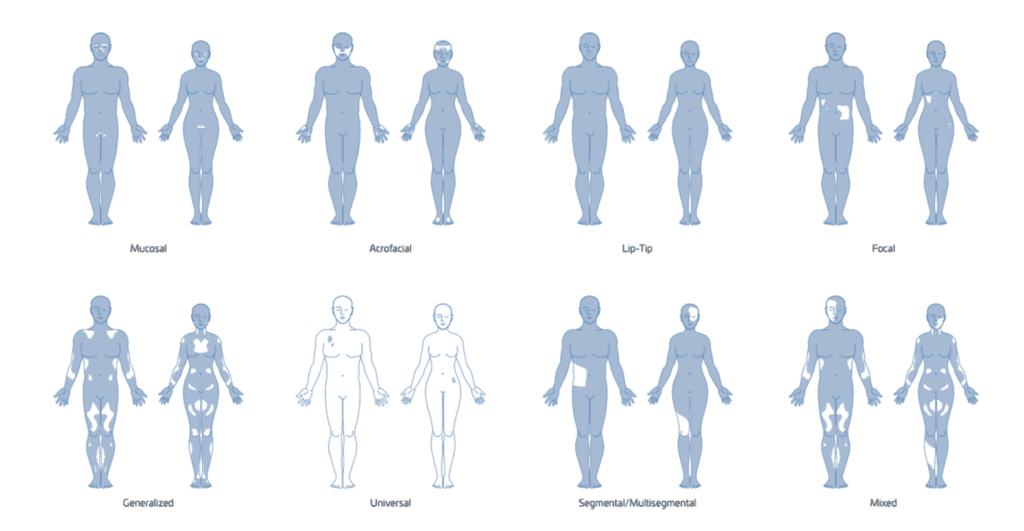
Image credit:https://www.umassmed.edu/vitiligo/blog/blog-posts1/2020/05/patterns-of-vitiligo/
Signs and symptoms of Vitiligo
The main sign of vitiligo is the presence of white or lighter patches on the skin surrounded by normal skin. Besides the loss of color, vitiligo may also cause other symptoms, such as3:
- Premature whitening or graying of the hair on the scalp, eyelashes, eyebrows, or beard
- Loss of color in the retina, which can lead to vision problems
- Sensitivity to sunlight or tanning beds
- Discoloration of the mucous membranes inside the mouth or nose
- Depigmentation of the skin around the mouth, nose, or eyes
Vitiligo can occur at any age but often begins in childhood or early adulthood. In some cases, it can remain stable or progress slowly; in others, it may progress rapidly.
Causes of Vitiligo
The exact cause of vitiligo is not fully understood, but several factors can increase your risk. These may include.4,7,8:
- Autoimmune response – Antibodies mistakenly target and destroy melanocytes
- Genetic factors – Inherited or mutated genes interrupt melanin production
- Environmental triggers – Extra time in the sun, chemical hazards, and viral infections
- Medications – Like drugs to treat hepatitis C, multiple sclerosis, and certain cancers
Unfortunately, autoimmune and genetic factors are unavoidable. With autoimmune responses, the body’s immune system mistakenly attacks and destroys melanocytes. If genetic factors cause vitiligo, your family history of vitiligo is often linked to specific genes that make you more likely to have it.
Environmental triggers and medications that affect the immune system are often avoidable. Those who work with chemicals should be careful to avoid getting any on their skin to lower tier risk. Also, if you need immune therapy, talk with your healthcare provider to discuss alternatives that won’t affect the skin.
Diagnosing Vitiligo
Diagnosing vitiligo involves reviewing your medical history, family history, and environmental exposures. Your healthcare provider will also look for changes to the skin and any symptoms you may be experiencing.
More tests may also be needed to confirm a diagnosis of vitiligo or rule out other conditions that can cause similar symptoms. These tests may include7,9:
This test uses a special lamp with ultraviolet (UV) light to help highlight areas of depigmentation on the skin. | |
Skin biopsy | A small sample of skin may be removed and examined under a microscope to look for changes in the pigmentation cells. |
Blood tests | These may be done to check for underlying autoimmune conditions that can be associated with vitiligo. |
A diagnosis may lead to further testing or referral to a skin specialist or dermatologist to discuss treatment options.
Treatment options for Vitiligo
Although there’s no known cure for vitiligo, various treatment options are available to manage the condition. You could also see improvement in the appearance of the affected skin. Medications applied to the skin or non-medicine-related techniques are currently available.
Medications applied to the skin may stop the progression of depigmentation, restore pigmentation, or depigment the skin (i.e., lighten the remaining pigmented areas until skin tone is even).11 The area of skin affected helps determine which medications are best.
Non-medication options typically involve restoring color to the skin using various techniques. Ultraviolet lights or lasers stimulate pigment-producing cells, while surgery or tattooing focuses on transplanting pigment-producing cells or adding pigment to the affected areas.11,12
It’s worth noting that the response to treatment can vary from person to person. Some treatments may have potential side effects or need ongoing maintenance. So, discussing the risks, benefits, and expected outcomes with a dermatologist or healthcare provider specializing in vitiligo treatment is key.
What to do if diagnosed?
Vitiligo is not contagious and poses no immediate health risks. But it can have a significant effect on self-esteem and quality of life.13 Joining support groups and counseling can be beneficial in helping individuals cope with emotional and social challenges.
Additionally, individuals with vitiligo need to protect their skin from sun exposure, which can lead to further damage. Using broad-spectrum sunscreen with a high SPF (30+), wearing protective clothing, and seeking shade during peak sunlight hours can help avoid further issues with vitiligo.14,15
The bottom line
Vitiligo is a skin condition affecting millions of people. But, for Black people, its effects are more than skin-deep. Uneven skin tones challenge the beauty standards we’ve set as a society. Join our community of support by sharing stories to raise awareness and advocate for inclusive representation across all aspects of life.
Conversation Starters:
- What did you find most interesting about vitiligo from this post?
- How have you seen individuals with vitiligo highlighted in the media/society?
- What other suggestions do you have to increase awareness around vitiligo?
References
- Gandhi, Kavita et al. “Prevalence of Vitiligo Among Adults in the United States.” JAMA dermatology vol. 158,1 (2022): 43-50. doi:10.1001/jamadermatol.2021.4724
- Cleveland Clinic. “Vitiligo of the Skin | Cleveland Clinic.” Cleveland Clinic, 2016, my.clevelandclinic.org/health/diseases/12419-vitiligo. Accessed 15 June 2023.
- Mayo Clinic. “Vitiligo – Symptoms and Causes.” Mayo Clinic, 2018, www.mayoclinic.org/diseases-conditions/vitiligo/symptoms-causes/syc-20355912. Accessed 15 June 2023.
- Ludmann, Paula. “Vitiligo: Overview.” American Academy of Dermatology Association., 29 June 2022, www.aad.org/public/diseases/a-z/vitiligo-overview. Accessed 15 June 2023.
- “Patterns of Vitiligo.” University of Massachusetts Medical School, 29 May 2020, www.umassmed.edu/vitiligo/blog/blog-posts1/2020/05/patterns-of-vitiligo/. Accessed 15 June 2023
- “What Is Vitiligo? | Causes, Signs, Symptoms, & More | Vitiligo Society.” The Vitiligo Society, https://vitiligosociety.org/about-vitiligo/#what-is-vitiligo. Accessed 15 June 2023.
- NIAMS. “Vitiligo.” National Institute of Arthritis and Musculoskeletal and Skin Diseases, 12 Apr. 2017, www.niams.nih.gov/health-topics/vitiligo. Accessed 15 June 2023.
- “Vitiligo: MedlinePlus Genetics.” Medlineplus, 24 Feb. 2022, medlineplus.gov/genetics/condition/vitiligo/#causes. Accessed 15 June 2023.
- “Diagnosing Vitiligo.” Nyulangone.orNYU Langone Health, nyulangone.org/conditions/vitiligo/diagnosis. Accessed 15 June 2023.
- “Vitiligo – Treatment.” Nhs.uk, 20 Oct. 2017, www.nhs.uk/conditions/vitiligo/treatment/. Accessed 15 June 2023.
- Kubelis-López, David Emmanuel et al. “Updates and new medical treatments for vitiligo (Review).” Experimental and therapeutic medicine vol. 22,2 (2021): 797. doi:10.3892/etm.2021.10229
- Petrou, Ilya. “Cellular Grafting in Vitiligo.” Www.dermatologytimes.com, vol. 43, Mar. 2022, pp. 48–48, www.dermatologytimes.com/view/cellular-grafting-in-vitiligo. Accessed 15 June 2023.
- Grimes, P E, and M M Miller. “Vitiligo: Patient stories, self-esteem, and the psychological burden of disease.” International journal of women’s dermatology vol. 4,1 32-37. 8 Jan. 2018, doi:10.1016/j.ijwd.2017.11.005
- “Vitiligo Discomfort Stops with Sunscreen Use.” American Academy of Dermatology Association., www.aad.org/public/diseases/a-z/vitiligo-discomfort-stops-with-sunscreen. Accessed 15 June 2023.
“Vitiligo: Tips for Managing.” American Academy of Dermatology Association., www.aad.org/public/diseases/a-z/vitiligo-self-care. Accessed 15 June 2023.
You Might Also Like:

These Chipotle Swaps Will Save Your Gut & Skin
If you’ve ever left Chipotle feeling a little bloated or noticed your skin flaring up the next day, you’re not imagining things. These simple swaps could help your gut and skin health thrive.

Is Your “Waterproof” Sunscreen Lying to You?
As we slather on sunscreen, many of us reach for those bottles proudly proclaiming “waterproof” or “water resistant.” But have you ever stopped to wonder what those claims truly mean?









