We’ve all likely seen the CDC ads encouraging people to quit smoking to prevent long-term complications like lung cancer. However, in stories like Geri M’s, smoking led her to develop chronic obstructive pulmonary disease, or COPD.
COPD is a progressive lung disease that affects millions of people worldwide.1 In 2020, it was the 6th leading cause of death for Americans.2 Women and Black people are affected more often, especially those with other chronic health conditions.3,4 Unfortunately, emergency room visits, hospitalizations, and death rates for Black people with COPD are higher than non-Hispanic whites.5
To lower your risk of developing COPD, you must understand your risk factors and what you can do to prevent their impact.
What is COPD?
COPD is a progressive and debilitating respiratory condition that does not have a cure. Generally, COPD encompasses a range of lung diseases, with the two most common including chronic bronchitis and emphysema (more about these below).6 Those with COPD have issues with airflow and difficulty breathing, limiting their ability to live an active lifestyle.
Understanding the complexities of COPD is crucial, as it highlights the need for early diagnosis, lifestyle changes, and appropriate management strategies to improve your quality of life and reduce the burden of this chronic condition.
Chronic Bronchitis
Chronic bronchitis occurs when your airways become inflamed repeatedly. Structurally your lungs are working, but the inflammation makes it difficult for air to pass through freely, leading to breathing problems.7
Emphysema
On the other hand, emphysema causes your lungs to undergo structural changes or tissue damage. If lung tissues are destroyed, they can no longer allow oxygen to pass through effectively, causing you to be short of breath easily.8
Signs and Symptoms of COPD
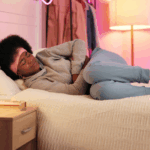
COPD poses significant challenges as it gradually impairs your ability to breathe. You may experience some or all of these symptoms, but they worsen as COPD progresses. Some common signs and symptoms of COPD include.1,9-12:
- Shortness of breath (dyspnea {disp·nee·uh})
- Chronic cough with mucus production
- Wheezing
- Chest tightness
- Fatigue
- Frequent respiratory infections
- Reduced exercise tolerance
- Unintended weight loss
- Bluish lips or fingernails (cyanosis {sai·yuh·now·suhs})
- Swelling in the ankles, feet, or legs
It’s important to note that these symptoms may vary in severity and overlap with other respiratory conditions. If you or someone you know is experiencing these symptoms, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate management.
Causes of COPD
Smoking is the primary cause of COPD, but nearly 30% of people with COPD have never smoked.13 In this group, it’s likely exposure to environmental factors such as air pollution and occupational hazards contributing to the development of COPD. In Black people, COPD can occur in those with a less extensive smoking history and at younger ages.5
For some, risk factors can’t be changed, like those over 40 years old, a history of asthma, or alpha-1 antitrypsin (AAT) protein deficiency leading to COPD. Additionally, some infectious diseases like HIV or tuberculosis, which also affect black people more often, can increase your risk of developing COPD due to their effects on the lungs.14-16
| Medical History | Your healthcare provider will ask about your symptoms, smoking history, exposure to environmental pollutants, occupational hazards, and any family history of lung disease. |
| Physical Exam | Your healthcare provider will listen to your lungs with a stethoscope and check for signs such as wheezing, prolonged expiration, and decreased breath sounds. |
| Lung Function Tests | Spirometry is the primary breathing test used to diagnose and assess the severity of COPD (and other lung diseases like asthma). It measures how much air you can inhale and exhale and how quickly you can exhale forcefully. |
| Imaging Studies | Chest X-rays and/or CT scans may be used to assess the extent of lung damage, rule out other conditions, and identify complications like lung infections or lung cancer. |
To best determine how to treat your COPD after diagnosis, it must first be staged based on the severity of your symptoms, lung function, and the impact on your daily life. Using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) system, you’ll be assigned one of four stages:
| Stage | Common symptoms at this stage |
| Stage 1 – Mild | Occasional cough and shortness of breath during physical exertion |
| Stage 2 – Moderate | Worsening airflow limitation, increased symptoms, and a greater impact on daily activities |
| Stage 3 – Severe | Further deterioration in lung function significantly impacting your quality of life and requiring more medical intervention |
| Stage 4 – Very Severe | Frequent flare-ups and a significant limitation in daily activities |
It’s important to note that the staging system helps your healthcare provider develop a plan, but each person’s experience with COPD can vary. Regular follow-ups with a healthcare provider are essential for monitoring the disease and adjusting the management plan.
Treatment options for COPD
Treatment options and recommendations for COPD depend on several factors. Your specific needs, preferences, comorbidities, stage of COPD, possible side effects, and affordability of medications all play a role. Recommended treatment options for COPD are18,19,:
- Short and long-acting bronchodilators: These medications help relax and open the airways, making breathing easier.
- Inhaled Corticosteroids: These medications help reduce airway inflammation and are generally used in individuals with more severe COPD or frequent flare-ups.
- Combination Medications: Combination inhalers containing long-acting bronchodilators and inhaled corticosteroids are commonly prescribed for moderate to severe COPD.
- Phosphodiesterase-4 (PDE-4) Inhibitors: These help reduce inflammation in the airways. They are usually prescribed for severe COPD with chronic bronchitis and a history of flare-ups.
- Theophylline: This helps when other treatments are ineffective or if cost is a factor. It works to improve breathing and prevent episodes of worsening COPD.
- Antibiotics: These treat or help prevent lung infections that worsen symptoms related to COPD.
More invasive treatment options may be needed for those with severe disease outside of medications. You could be placed on oxygen or recommended for surgery, such as a lung transplant. It’s recommended to consult with a healthcare provider, preferably a pulmonologist or respiratory specialist, who can provide personalized recommendations based on your COPD severity, symptoms, and overall health status.
What to do if diagnosed?
Once diagnosed, it’s vital to slow COPD progression as much as possible. A few ways to help preserve your current lung function and prevent further complications include18:
- Taking medications as directed
- Pulmonary rehabilitation
- Developing self-management strategies
- Avoiding triggers
- Seeking emotional and social support
- Attending regular follow-ups
Adopting certain lifestyle choices and avoiding exposure to risk factors is key to managing your COPD. Lifestyle modifications proven to be effective include19:
- Avoiding tobacco smoke
- Minimizing exposure to pollutants
- Getting vaccines (flu and pneumonia)
- Exercising regularly
- Eating a balanced diet
Remember, COPD is a chronic condition, but you can slow its progression and lead a fulfilling life with proper management and lifestyle changes. By implementing these actionable steps and working closely with your healthcare team, you can optimize your lung health and improve your overall well-being.
Resources:
- World Health Organization. “Chronic Obstructive Pulmonary Disease (COPD).” World Health Organization: WHO, 16 Mar. 2023, www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd) . Accessed 9 June 2023.
- Syamlal, Girija, et al. “Chronic Obstructive Pulmonary Disease Mortality by Industry and Occupation — United States, 2020.” MMWR. Morbidity and Mortality Weekly Report, vol. 71, no. 49, 2022, https://doi.org/10.15585/mmwr.mm7149a3. Accessed 9 June 2023.
- Centers for Disease Control and Prevention. “National Trends – Chronic Obstructive Pulmonary Disease (COPD) | CDC.” Centers for Disease Control and Prevention, 11 July 2022, www.cdc.gov/copd/data-and-statistics/national-trends.html. Accessed 9 June 2023.
- Nirupama Putcha, M. D., et al. “Comorbidities of COPD Have a Major Impact on Clinical Outcomes, Particularly in African Americans.” Chronic Obstructive Pulmonary Diseases:Journal of the COPD Foundation, vol. 1, no. 1, May 2014, pp. 105–14, journal.copdfoundation.org/jcopdf/id/1028/Comorbidities-of-COPD-Have-a-Major-Impact-on-Clinical-Outcomes-Particularly-in-African-Americans. Accessed 9 June 2023.
- Ejike, Chinedu O et al. “Chronic Obstructive Pulmonary Disease in America’s Black Population.” American journal of respiratory and critical care medicine vol. 200,4 (2019): 423-430. doi:10.1164/rccm.201810-1909PP. Accessed 9 June 2023.
- National Heart, Lung, and Blood Institute. “COPD – What Is COPD? | NHLBI, NIH.” National Institute of Health, 24 Mar. 2022, www.nhlbi.nih.gov/health/copd. Accessed 9 June 2023.
- National Institute of Health. “Bronchitis | NHLBI, NIH.” National Institute of Health , 2 Dec. 2022, www.nhlbi.nih.gov/health/bronchitis. Accessed 9 June 2023.
- Mayo Clinic. “Emphysema – Symptoms and Causes.” Mayo Clinic, 28 Apr. 2017, www.mayoclinic.org/diseases-conditions/emphysema/symptoms-causes/syc-20355555. Accessed 9 June 2023.
- Centers for Disease Control and Prevention. “CDC – Basics about COPD – Chronic Obstructive Pulmonary Disease (COPD).” Centers for Disease Control and Prevention, 19 July 2019, www.cdc.gov/copd/basics-about.html#anchor_1510688168948. Accessed 11 June 2023.
- National Institute of Health. “COPD – Symptoms | NHLBI, NIH.” National Institute of Health, 24 Mar. 2022, www.nhlbi.nih.gov/health/copd/symptoms. Accessed 11 June 2023.
- American Lung Association. “COPD Symptoms.” American Lung Association, 5 Mar. 2021, www.lung.org/lung-health-diseases/lung-disease-lookup/copd/symptoms-diagnosis. Accessed 11 June 2023.
- NHS . “Symptoms – Chronic Obstructive Pulmonary Disease (COPD).” NHS, 2019, www.nhs.uk/conditions/chronic-obstructive-pulmonary-disease-copd/symptoms/. Accessed 11 June 2023.
- National Institute of Health. “Lung Development May Explain Why Some Non-Smokers Get COPD and Some Heavy Smokers Do Not.” National Institutes of Health (NIH), 9 June 2020, www.nih.gov/news-events/news-releases/lung-development-may-explain-why-some-non-smokers-get-copd-some-heavy-smokers-do-not#:~:text=%E2%80%9CThis%20helps%20us%20to%20understand. Accessed 9 June 2023.
- HIV.gov. “HIV Statistics Impact on Racial and Ethnic Minorities.” HIV.gov, 20 Jan. 2023, www.hiv.gov/hiv-basics/overview/data-and-trends/impact-on-racial-and-ethnic-minorities/. Accessed 12 June 2023.
- CDCTB. “TB and Black or African American Persons.” Centers for Disease Control and Prevention, 25 Oct. 2021, www.cdc.gov/tb/topic/populations/tbinafricanamericans/default.htm#:~:text=The%20rate%20of%20TB%20disease. Accessed 12 June 2023.
- National Heart, Lung, and Blood institute. “COPD – Causes and Risk Factors | NHLBI, NIH.” National Heart, Lung, and Blood institute, 24 Mar. 2022, www.nhlbi.nih.gov/health/copd/causes. Accessed 12 June 2023.
- National Heart, Lung, and Blood institute. “COPD – Diagnosis | NHLBI, NIH.” National Heart, Lung, and Blood institute, 24 Mar. 2022, www.nhlbi.nih.gov/health/copd/diagnosis#:~:text=The%20main%20test%20for%20COPD. Accessed 11 June 2023.
- American Lung Association. “Understanding Your COPD Medications.” American Lung Association, 28 Apr. 2023, www.lung.org/lung-health-diseases/lung-disease-lookup/copd/treating/copd-medications. Accessed 12 June 2023.
- Mayo Clinic. “COPD – Diagnosis and Treatment – Mayo Clinic.” Mayo Clinic, 15 Apr. 2020, www.mayoclinic.org/diseases-conditions/copd/diagnosis-treatment/drc-20353685. Accessed 12 June 2023.
Join Our Community
Get active in a community that understands you, wants to hear about your health and wellness, and informs you of information and opportunities to keep you and other people of color healthy.
You Might Also Like:

5 Heart-Pumping Workouts to Kickstart Your New Year
The new year is often a time for fresh starts and resolutions – start yours with these heart-healthy exercises.

Post Holiday Detox Diet and How to Stick to It
A post-holiday detox diet isn’t about punishing yourself or giving up everything you love. It’s about fueling your body with what it needs to feel good again. Learn more.