Living with a chronic condition like myasthenia gravis (MG) often means navigating a world of uncertainty—one where even simple daily tasks can feel unpredictable. MG is a rare autoimmune neuromuscular condition that disrupts the communication between nerves and muscles, leading to symptoms like muscle weakness, drooping eyelids, difficulty swallowing, and fatigue that can worsen with activity.
It affects people of all ages, but most commonly strikes women under 40 and men over 60. Because symptoms can vary widely and fluctuate throughout the day, MG can be both physically and emotionally exhausting—not just for those diagnosed, but also for their families and caregivers.
With no obvious cause and no clear cure, it’s only natural that the question looms large for anyone facing this diagnosis: Is myasthenia gravis curable? In this article, we’ll explore the current science, treatment options, and the hope that continued research brings to the MG community.
Understanding Myasthenia Gravis (MG)
MG is a chronic neuromuscular disease that causes weakness in the voluntary muscles—the muscles you consciously control to move your body, make facial expressions, breathe, and swallow.1
MG is an autoimmune disease, which means your body’s defense system mistakenly attacks healthy cells. In this case, your immune system targets the connection point between nerves and muscles.1
The onset can be sudden, and symptoms might not be immediately recognized as myasthenia gravis. The degree of muscle weakness varies greatly from person to person.1
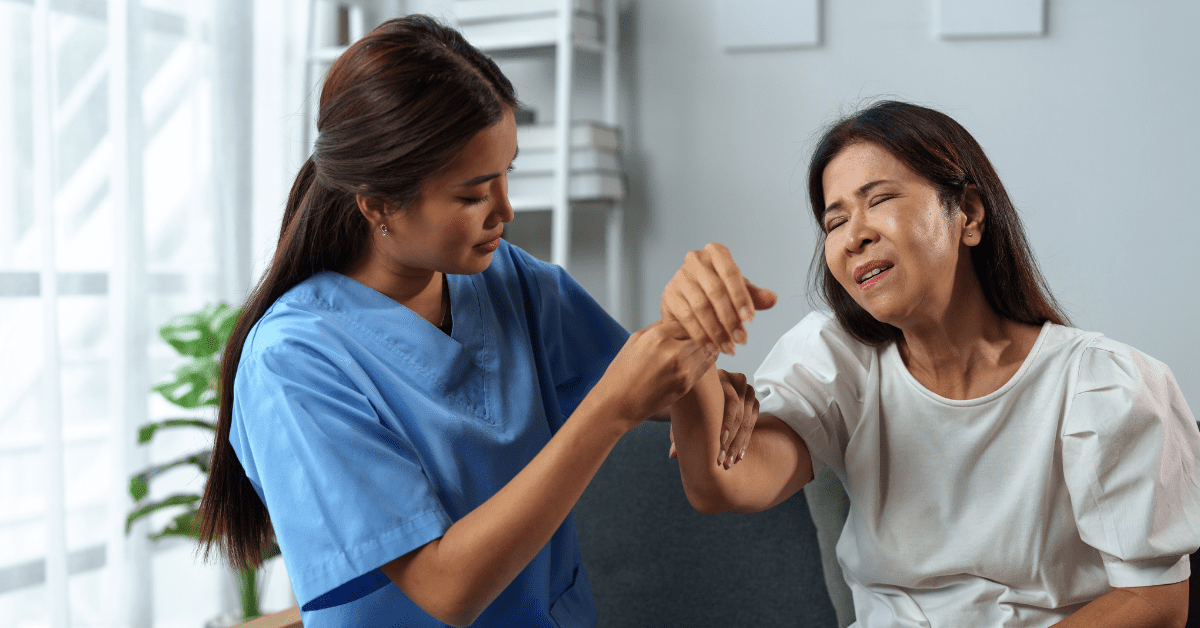
Common Symptoms
People with myasthenia gravis may experience:1
- Weakness of the eye muscles (ocular myasthenia)
- Drooping of one or both eyelids (ptosis)
- Blurred or double vision (diplopia)
- Changes in facial expressions
- Difficulty swallowing
- Shortness of breath
- Impaired speech (dysarthria)
- Weakness in the arms, hands, fingers, legs, and neck
In some cases, the muscles that control breathing can weaken severely, leading to a “myasthenic crisis” that requires immediate emergency care. This crisis might be triggered by infection, stress, surgery, or medication reactions—though many people can’t identify what triggered their crisis.1
Who Gets Myasthenia Gravis (MG)?
MG affects both men and women across all racial and ethnic groups. It most commonly impacts:1
- Young adult women (under 40)
- Older men (over 60)
However, it can occur at any age, including childhood. MG is neither inherited nor contagious, though occasionally it may affect multiple members of the same family.
What Causes Myasthenia Gravis (MG)?
At its core, MG disrupts how nerve signals are sent to muscles. Here’s what happens:1
- Normally, when your brain sends a signal to move a muscle, nerve endings release a chemical called acetylcholine
- This chemical binds to receptors on the muscle, telling it to contract
- In myasthenia gravis, antibodies block, alter, or destroy these receptors
- As a result, the message from the nerve doesn’t properly reach the muscle
The thymus gland, which controls immune function, often plays a role in MG. Many adults with myasthenia gravis have an abnormally large thymus gland, and some develop thymus tumors called thymomas. Scientists believe the thymus may give incorrect instructions to developing immune cells, causing them to attack the body’s own tissues.1
Diagnosing Myasthenia Gravis (MG)
Doctors use several tests to confirm myasthenia gravis:
- Physical and neurological examination to check muscle strength, coordination, sense of touch, and eye movements.1
- Electrodiagnostic tests including:
- Repetitive nerve stimulation, which uses small pulses of electricity to test muscle responses
- Single fiber electromyography (EMG), considered the most sensitive test for detecting MG
- Blood tests to check for abnormally elevated levels of certain antibodies. Some people have “seronegative” myasthenia, meaning these antibodies aren’t detectable in their blood.1
Diagnosis can be challenging, especially in people with mild or limited muscle weakness, as weakness is a common symptom of many conditions.1
Current Treatments
Currently, there is no known cure for myasthenia gravis (MG). However, most people with MG have a normal life expectancy. Several treatments can help reduce and improve muscle weakness:1
- Anticholinesterase medications like mestinon or pyridostigmine, which slow the breakdown of acetylcholine and improve muscle strength.
- Thymectomy – surgical removal of the thymus gland, which can reduce symptoms by potentially rebalancing the immune system. About 50% of people who undergo this procedure may achieve stable, long-lasting complete remissions.
- Complement inhibition medications like eculizumab, which target proteins involved in the immune response that damage the connection between nerves and muscles.
- Immunosuppressive drugs like prednisone, azathioprine, mycophenolate mofetil, and tacrolimus, which suppress the production of abnormal antibodies, but require careful monitoring due to potential side effects.
- Emergency treatments for severe cases:
- Plasmapheresis – uses a machine to remove harmful antibodies from blood plasma.
- Intravenous immunoglobulin – concentrated antibodies from healthy donors that temporarily modify immune system function.
- Lifestyle changes – Regular gentle exercise may benefit some people with MG.
- Assistive devices to help with mobility.
Remission Possibilities
Some cases of myasthenia gravis (MG) may go into remission, either temporarily or permanently. When this happens, muscle weakness may disappear completely, allowing some people to stop taking medications (after consulting with their doctor).2
Thymectomy surgery may lead to stable, long-lasting complete remissions in about 50% of those who undergo the procedure.2
Research Progress
Although there is no cure yet, management of myasthenia gravis (MG) has improved significantly over the past 30 years. Researchers continue to:2
- Develop better medications
- Identify new diagnostic and treatment approaches
- Improve existing treatment options
The National Institute of Neurological Disorders and Stroke (NINDS) and other research organizations continue to support research to better understand the causes of MG and develop more effective treatments.2
Living with Myasthenia Gravis (MG)
With proper treatment, most people with MG can significantly improve their muscle weakness and lead normal or nearly normal lives. While it remains a chronic condition without a cure at present, ongoing advances in understanding and treating MG continue to improve the outlook for those living with this condition.
References
- NIH. ( 2024, July 19). Myasthenia Gravis. Retrieved from National Institute of Neurological Disorders and Stroke: https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis
- NIH. (2020, March). Myasthenia Gravis. Retrieved from National Institute of Neurological Disorders and Stroke: https://www.ninds.nih.gov/sites/default/files/migrate-documents/myasthenia_gravis_e_march_2020_508c.pdf
You Might Also Like:
Is It Anxiety or a Rare Muscle Disorder?
While anxiety can absolutely cause physical symptoms, some signs may point to something deeper, like myasthenia gravis (MG)—a rare, often misunderstood neuromuscular disorder. Learn more.