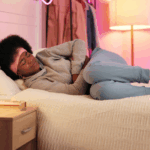
Navigating a chronic condition like ulcerative colitis (UC) can feel like a constant battle. This inflammatory bowel disease (IBD) causes inflammation in the large intestine, leading to debilitating symptoms like bloody stools, urgent and frequent trips to the bathroom, and persistent pain.1 These aren’t just minor inconveniences; they are significant disruptions that can severely diminish a person’s quality of life.1
While modern therapies such as biologics and immunomodulators have brought relief to many, they aren’t effective for everyone.2 For roughly one in three people with UC, medication eventually fails to control the condition.2 At this point, surgery may be the only remaining option.
For some, this decision is made suddenly as a life-saving measure in the hospital, while for others, it’s a planned choice to reclaim their life before UC completely takes over.2
This reality highlights the need to look beyond symptoms alone. Understanding the necessity of surgery for UC involves examining the intricate ways the disease affects the digestive system, the body’s inflammatory response, and the healthcare disparities that can influence who requires surgery and when.
The Digestive Tract and Ulcerative Colitis (UC)
The large intestine plays a crucial role in absorbing water, forming stool, and supporting immune defense. In UC, inflammation begins in the rectum and often spreads continuously through the colon.3
This inflammation damages the mucosal lining, disrupts barrier function, and sets off cycles of pain, bleeding, and urgency. Unlike Crohn’s disease, which causes patchy lesions, UC’s continuous involvement makes the colon especially vulnerable to structural and functional compromise.3
The Inflammatory Response in Ulcerative Colitis (UC)
At its core, UC is the result of the immune system going off balance. The “good” bacteria in the gut shift, the cells that normally keep inflammation in check lose control, and certain chemical messengers, like TNF-α and IL-13, fuel ongoing damage.4
Inside the colon, this constant attack wears down the lining, creating open sores (ulcers), pockets of infection, and even growths called pseudopolyps.4 But UC doesn’t always stop there. In some people, the inflammation spreads beyond the gut, triggering arthritis, skin rashes, or even eye problems.4
And because the colon is under constant stress, long-term inflammation raises the risk of precancerous changes and colorectal cancer.4
Disparities in Ulcerative Colitis (UC) Care
Not every person has the same journey with UC. Research shows that Black, Hispanic, and people in rural locations often experience delays in diagnosis and less access to advanced therapies.5 Insurance status and socioeconomic barriers can make long-term biologic therapy financially out of reach, forcing reliance on steroids or older medications.5
As a result, these groups are more likely to present with severe disease requiring emergency surgery, a scenario that carries higher risks and worse outcomes compared to planned, elective surgery.5 Addressing these inequities is critical to improving outcomes across all communities.
When May Surgery be an Option?
Surgery for ulcerative colitis (UC) is not taken lightly, but it is sometimes the best or only option. Surgery for ulcerative colitis may be an option in a few key situations:
- Emergency Situations: This happens when a person’s condition becomes life-threatening. This includes severe bleeding, a hole in the bowel (bowel perforation), or a dangerous widening of the colon (toxic megacolon). In these cases, surgery is needed immediately.2
- Ongoing, Severe Symptoms: For people with chronic UC, surgery may be the best option when medications no longer control symptoms like pain, diarrhea, and bleeding. This is often the case for those who have become dependent on steroids, as long-term use can have serious side effects.2
- Preventing Cancer: Over time, long-standing UC can increase the risk of colon cancer. Surgery might be recommended if precancerous cells or cancer itself are found in the colon.2
What Happens During Surgery?
The most common surgery for UC is called a total proctocolectomy with ileal pouch-anal anastomosis (IPAA). In this procedure, the surgeon removes your entire colon and rectum. They then create a new pouch from the end of your small intestine, which acts as a new rectum. This allows you to pass stool in a more typical way.
If you have an emergency, a different procedure may be done first to stabilize you. This involves removing the colon but leaving the rectum. The end of the small intestine is brought through the abdominal wall to create a temporary opening, or ileostomy, where waste is collected in a bag. A second surgery may be performed later to create the internal pouch.
Your Quality of Life Matters
Surgery is not the first-line treatment for ulcerative colitis, but it is often a life-saving or life-enhancing option when other therapies fail.
Knowing the circumstances under which surgery becomes necessary can ease fear and foster informed choices. For healthcare systems, addressing disparities in diagnosis, treatment access, and surgical timing is crucial. In the end, surgery for UC represents both a last resort and a new beginning; restoring health, function, and hope.
References
- Crohn’s & Colitis Foundation. (2025). What is Ulcerative Colitis? Retrieved from Crohn’s & Colitis Foundation: https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis
- Crohn’s & Colitis Foundation. (2025). Surgery for Ulcerative Colitis. Retrieved from Crohn’s & Colitis Foundation: https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-ulcerative-colitis/surgery
- CDC. (2024, June 21). Ulcerative Colitis Basics. Retrieved from Centers for Disease Control and Prevention: https://www.cdc.gov/inflammatory-bowel-disease/about/ulcerative-colitis-uc-basics.html
- Kałużna, A., Olczyk, P., & Komosińska-Vassev, K. (2022). The Role of Innate and Adaptive Immune Cells in the Pathogenesis and Development of the Inflammatory Response in Ulcerative Colitis. Journal of Clinical Medicine. doi:10.3390/jcm11020400
- Burbage, S. C., Krupsky, K. L., Cambron-Mellott, M. J., Way, N., Patel, A. A., & Liu, J. J. (2024). Patient-Reported Racial and Ethnic Disparities in Patients With Ulcerative Colitis: Results From the National Health and Wellness Survey. Crohn’s & Colitis 360. doi:10.1093/crocol/otae048