Your brain is the command center for everything, from recalling cherished memories to making decisions, feeling emotions, and recognizing loved ones. Alzheimer’s disease, the most common form of dementia, affects over 6 million Americans, and that number is rising as our population ages.1 But Alzheimer’s is not just “memory loss.” It’s a progressive neurological condition that slowly wears away brain function, changing who we are and how we connect with the world.1
This article will explain how a healthy brain works, what happens in Alzheimer’s, who’s at risk, and most importantly, what you can do right now to support your brain’s health.
How a Healthy Brain Works
The human brain is a complex and dynamic system made up of approximately 86 billion neurons. These specialized cells communicate with each other using chemicals called neurotransmitters, which help transmit signals necessary for everything from memory to movement.
One of the most important neurotransmitters for learning and memory is acetylcholine. This chemical supports the work of critical brain regions like the hippocampus (responsible for forming new memories), and the cerebral cortex (which handles reasoning, language, and decision-making).2
To function properly, neurons need a consistent supply of oxygen-rich blood and glucose, which fuels the brain’s activity. When this system is healthy and intact, your brain works seamlessly: you think clearly, recall information with ease, and navigate daily life with purpose and identity. But when these systems break down, cognition begins to deteriorate, opening the door to neurodegenerative diseases like Alzheimer’s.2
What is Alzheimer’s Disease?
Alzheimer’s disease is a progressive neurological disorder that disrupts the brain’s ability to function normally. It begins subtly, often with mild forgetfulness, but gradually causes significant memory loss, confusion, and personality changes. Unlike normal aging, Alzheimer’s is driven by pathological changes in brain structure and chemistry.3
Two hallmark features of Alzheimer’s are amyloid plaques and tau tangles. Amyloid plaques are clumps of protein fragments that build up in the spaces between neurons, interfering with cell-to-cell communication. Tau tangles, on the other hand, are twisted fibers of the tau protein that form inside neurons, blocking the transport of nutrients and essential molecules within the cell. These abnormalities lead to neuron dysfunction and eventual cell death.3
Who’s at Risk & Why it Matters
Age:
Age is the most significant risk factor for Alzheimer’s. After age 65, your risk roughly doubles with each five-year increment—and by age 85, nearly one-third of individuals are affected. While aging alone doesn’t cause Alzheimer’s, the passage of time allows disease-related changes, like amyloid plaques and tau tangles, to accrue and harm the brain’s structure and function.4
Genetics:
Genetics also play a major role. One key gene, APOE ε4, increases Alzheimer’s risk in a dose-dependent manner: people with one copy face about a threefold increased risk, while those with two copies may have up to a 15‑fold higher risk, and up to 60% of such individuals may develop dementia by age 85. Yet genetics aren’t destiny: many carriers never develop the condition, and people without these variants sometimes do.4
Chronic Conditions:
Beyond non‑modifiable factors, several health and lifestyle issues significantly raise risk. High blood pressure, diabetes, obesity, smoking, and elevated cholesterol, all of which impair blood vessels and oxygen delivery to the brain, are linked to increased dementia rates. Alarmingly, studies suggest that up to 45% of dementia cases might be prevented or delayed by addressing lifestyle factors, such as inactivity, smoking, hearing loss, social isolation, and poor diet, at the right times during life.4
Symptoms to Watch For
Alzheimer’s typically begins with subtle changes, but recognizing early signs can make a significant difference:
-
Early-stage signs include routine forgetfulness or struggling to recall recent events or conversations.5
-
As it progresses, individuals may become disoriented about time or place, struggle with planning tasks, and experience mood shifts or anxiety.5
-
In moderate stages, memory loss becomes more frequent; repeated questions and difficulty managing daily routines (like dressing or cooking) are common.5
- In advanced stages, independence wanes. Individuals may lose the ability to communicate, require full-time assistance, and become vulnerable to infections.5
Managing Alzheimer’s
Though there’s no cure yet, interventions can improve quality of life:
-
Medications such as donepezil and memantine can help stabilize symptoms in early to moderate stages.6
-
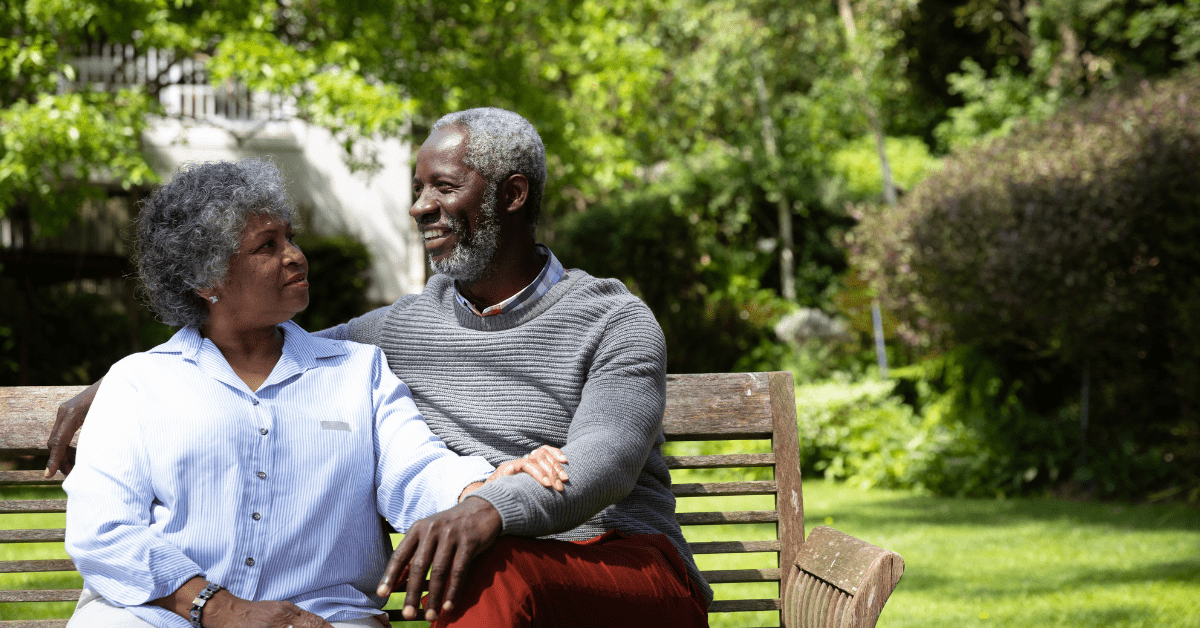
Lifestyle strategies, including structured daily routines, physical exercise, mental stimulation (e.g., puzzles or learning), and ongoing social engagement, support cognitive function.6
- Caregiver support is equally essential, through counseling, respite care, and community programs, to help reduce burden and enhance care effectiveness.6
What You Can Do Now
-
Support Heart & Vascular Health
Keeping blood pressure, cholesterol, and blood sugar in check isn’t just smart for your cardiovascular (heart) system—it’s protective for your brain. Addressing high blood pressure in midlife may lower dementia risk by up to 15%.7
-
Be Physically Active
Regular aerobic exercise, such as walking, swimming, or cycling, boosts blood flow, builds new neural connections, and helps clear abnormal proteins from the brain. Research shows active individuals may reduce their Alzheimer’s risk by about 76%.7
-
Eat for Brain Health
Diets like the mediterranean or MIND diet, rich in vegetables, fruits, whole grains, nuts, lean fish, and healthy oils, have been linked to a 35–53% lower risk of dementia.7
-
Engage Your Mind
Activities that challenge your brain, reading, learning a new skill, or language, solving puzzles, help build cognitive resilience (“reserve”), which may delay symptom onset.7
-
Sleep and Stress Matter
Quality sleep allows the brain to flush out toxins like amyloid-beta; chronic stress leads to inflammation both physically and in the brain, accelerating damage.7
Conclusion
Alzheimer’s is complex, but it isn’t helpless. Early knowledge, proactive changes, and community support can redefine the journey. Every movement, meal, mental challenge, and medical check-in matters, because your brain’s future is shaped by what you do today.
And for every person living with Alzheimer’s, small steps now can protect a lifetime’s worth of memories.
References
- NIH. (2023, April 5). Alzheimer’s Disease Fact Sheet. Retrieved from NIH – National Institute on Aging: https://www.nia.nih.gov/health/alzheimers-and-dementia/alzheimers-disease-fact-sheet
- NIH. (2025, February 25). Brain Basics: Know Your Brain. Retrieved from National Institute of Neurological Disorders and Stroke: https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-know-your-brain
- NIH. (2024, January 19). What Happens to the Brain in Alzheimer’s Disease? Retrieved from NIH National Institute on Aging: https://www.nia.nih.gov/health/alzheimers-causes-and-risk-factors/what-happens-brain-alzheimers-disease
- Alzheimer’s Association. (2025). What are the Causes and Risk Factors of Alzheimer’s and Other Dementias? Retrieved from Alzheimer’s Association: https://www.alz.org/alzheimers-dementia/what-is-alzheimers/causes-and-risk-factors
- Alzheimer’s Association. (2025). 10 Early Signs and Symptoms of Alzheimer’s and Dementia. Retrieved from Alzheimer’s Association: https://www.alz.org/alzheimers-dementia/10_signs
- Alzheimer’s Association. (2025). Treatments for Alzheimer’s. Retrieved from Alzheimer’s Association: https://www.alz.org/alzheimers-dementia/treatments
- CDC. (2024, August 27). Reducing Risk for Dementia. Retrieved from Centers for Disease Control and Prevention: https://www.alz.org/alzheimers-dementia/treatments