Some say beauty is only skin deep, but what do you do if you have a skin condition that challenges what’s been historically accepted as the “standard of beauty”?
Skin conditions affect millions of people worldwide. However, they appear differently in people of various racial and ethnic backgrounds, especially Black people. From conditions like eczema to hidranitis suprativa, these conditions can significantly impact physical health and self-esteem.
Recognizing the unique challenges of some skin conditions helps empower individuals with the knowledge to better address and manage them. Let’s explore some common skin conditions affecting Black people.
Common Skin Conditions
Many skin conditions are seen across all types of people, but some occur more often or show up differently in Black people. You may have heard of some of these skin conditions, while others, like prurigo nodularis, may leave you wondering what exactly it is.
Eczema
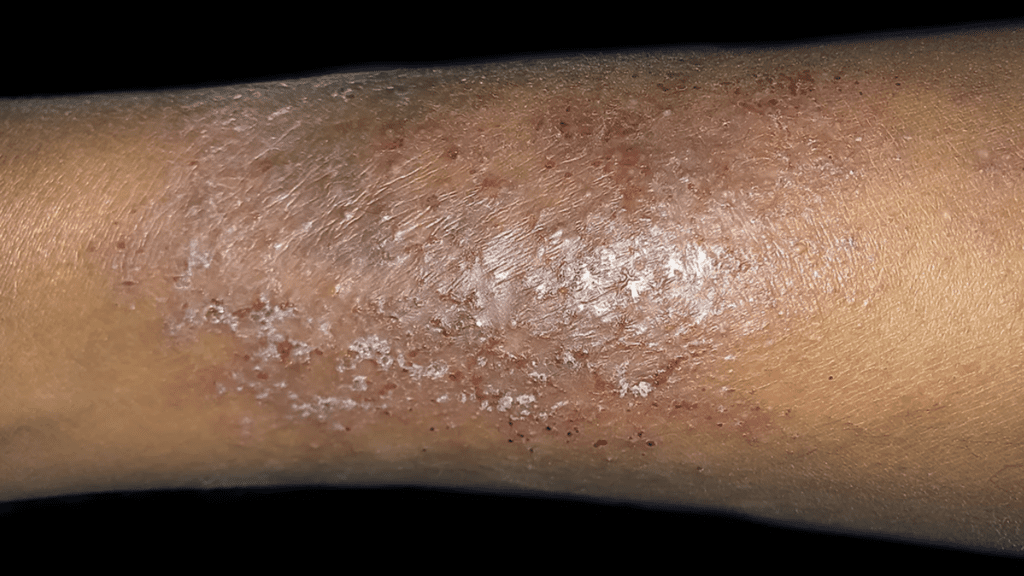
Eczema (atopic dermatitis) is a chronic condition causing the skin to be red, itchy, and inflamed. On Black people, these areas could appear darkened or even lighter due to inflammation and damage to the cells responsible for skin color, or melanin.
For some Black people, eczema appears as ashy or gray patches on the skin, particularly in areas that repeatedly flare up. In more severe cases, these patches become raised or blister and may ooze or crust over. With time, the skin becomes thickened and develops cracks. This is more noticeable on darker skin tones.
Studies in the United States have shown that eczema is more commonly diagnosed in Black people than in other racial or ethnic groups.1 The reasons for these variations are complex and may be influenced by genetic, environmental, and socioeconomic factors.
Eczema Triggers
While the underlying causes of eczema are not fully understood, some common triggers are seen among individuals with darker skin tones. These include:
- Dry Skin: Environmental factors like low humidity can contribute to dry skin.
- Irritants: Harsh soaps, detergents, and certain fabrics can irritate the skin and worsen eczema symptoms.
- Allergens: Pollen, pet dander, dust mites, and specific food triggers eczema flare-ups.
- Stress: Emotional stress or anxiety can lead to worsening of eczema symptoms.
- Heat and Sweat: Excessive heat and sweating can aggravate eczema, particularly in areas prone to friction and sweating.
- Fragrances and Chemicals: Some perfumes, colognes, and chemicals in skincare or household products can be irritating.
What triggers one person’s flare-up may not affect another similarly. Finding out your triggers can make managing eczema a lot easier.
Treatment options for Eczema
There is no cure for eczema. Treatment and management of eczema focuses on alleviating symptoms, preventing flare-ups, and improving overall skin health.
Many treatment options are applied directly to the skin to help reduce inflammation, itching, and redness. But what if you’re looking for treatment options that don’t include medications? Your options may surprise you2:
- Emollients (Moisturizers): Regularly applying a thick, fragrance-free moisturizer helps lock in moisture and prevent dryness, reducing the risk of irritation.
- Wet Wrap Therapy: Apply a moisturizer to the affected areas and then cover them with wet bandages or clothing to lock in moisture. This is particularly effective for severe cases.
- Bathing Habits: Take short, lukewarm baths or showers using mild, fragrance-free soap to help maintain skin moisture.
- Avoiding Triggers: Identify and avoid triggers that worsen eczema where possible.
- Allergy Shots: Regular injections of allergens in gradually increasing doses help your immune system recognize and reduce allergic reactions over time.
- Behavioral Strategies: Stress and anxiety worsen eczema, so stress management techniques such as meditation, yoga, or therapy are helpful.
Finding a healthcare professional or dermatologist specializing in treating skin conditions affecting Black people can help tailor your treatment plan to meet your needs.

Psoriasis
Psoriasis (sor·ai·uh·suhs) mainly affects the outermost layer of the skin or epidermis. In a healthy skin cycle, cells in the epidermis are produced and shed in about a month.
However, this process happens much quicker in psoriasis, leading to the rapid buildup of skin cells that form thick, scaly patches on the skin’s surface. It’s important to note psoriasis isn’t contagious and will come and go.
Nearly 2% of Black people in the US have psoriasis.3 Like eczema, psoriasis may look more light to dark brown, purple, or gray on darker skin vs. red or pink on lighter skin. Unfortunately, detecting psoriasis in people with darker skin may be more challenging as it could be confused with other skin conditions.
Black people may also have thicker areas of psoriasis, which take longer and are more challenging to treat. While psoriasis can affect any body part, Black people appear to have more common lesions on the scalp and cover larger areas of the body.
Types of Psoriasis
The type of psoriasis you have may also affect where and how it appears on your skin. The table below details each type of psoriasis and how it commonly appears.
Plaque Psoriasis | This is the most common type, characterized by raised, red patches covered with silvery-white scales. |
Guttate (guht-eyt) Psoriasis | Small, dot-like lesions develop on the skin, often triggered by bacterial infections or stress. |
Inverse Psoriasis | Smooth, red patches form in skin folds like the armpits, groin, and under the breasts. |
Pustular Psoriasis | White, pus-filled blisters surrounded by red skin, often on the hands and feet. |
Erythrodermic Psoriasis | This is a rare and severe form, where the skin becomes red, inflamed, and sheds scales. |
Treatment Options for Psoriasis
How psoriasis is treated depends on the type and location of the areas affected. Creams and lotions applied directly to the areas of psoriasis on the skin are used first. If you need additional treatment options your healthcare provider may recommend medications taken by mouth or injections.
Treating psoriasis in Black people can be challenging. In some cases, stronger topical creams and lotions are required. If topical medications don’t work well enough, your healthcare provider may recommend photo or light therapy. Unfortunately, phototherapy could cause more darkening or lightening of treatment areas.
How effective a treatment is varies from person to person. Working closely with a dermatologist is recommended to find the most suitable approach for your situation. They can provide personalized advice and monitor your progress.

Vitiligo
Vitiligo is a skin condition where the loss of melanin-producing cells in certain areas of the skin results in white patches. It’s particularly noticeable in people with darker skin tones, making it a source of self-consciousness.
Like other skin conditions, there are different types of vitiligo. A healthcare provider can tell you which kind you have based on its location, distribution, and progression. You will find more information on some common types of vitiligo here.
Vitiligo Causes and Triggers
Vitiligo’s exact cause is unclear, but certain factors can increase the likelihood of developing it. These include autoimmune responses, where the immune system mistakenly attacks and destroys melanin-producing cells. Inherited or mutated genes that disrupt melanin production could also be a factor.
Environmental triggers like prolonged sun exposure, exposure to chemicals, and viral infections can also play a role. Additionally, specific medications used to treat conditions such as hepatitis C, multiple sclerosis, and certain cancers can cause or worsen vitiligo.
Treatment options for Vitiligo
Like many other skin conditions, there’s no cure for vitiligo. Treatment options available work to even out your skin tone by increasing or decreasing its color.
Ironically, some of the same medications and non-medication-related techniques used to treat other skin conditions also work for vitiligo. Choosing the right treatment option for your skin depends on the location and size of vitiligo.
As always, talking with your healthcare provider or dermatologist about your options is essential.

Prurigo Nodularis (PN)
Prurigo nodularis is a rare, chronic skin condition that causes an intense itchy, hard, and crusty rash. A PN rash often appears on the same spot on the arms and legs but can occur anywhere on the body. It can last as long as six weeks, but sometimes will come and go over time.
The exact cause of PN is not well understood, but it’s believed to be related to chronic scratching or rubbing of the skin. It’s typically worsened by sweat, heat, clothing, and stress.
Anyone can have PN, but it’s most commonly seen in middle-aged and older adults, especially women.8 In one study, Black people were 3.4 times more likely to have PN.9 Some think this is because Black people are more likely to have conditions associated with PN, including:
- Eczema (Atopic Dermatitis)
- Chronic Kidney Disease
- Hepatitis C
- HIV/AIDS
- Diabetes
- Psychiatric Disorders (depression, anxiety, or obsessive-compulsive disorder)
The intense itching associated with this condition can significantly impact a person’s quality of life. It often leads to a cycle of itching and scratching, which worsens PN and can lead to infections.
Treatment options for PN
Up until September 2022, there wasn’t a medication approved for treating PN. Many of the options available to treat PN are used in other skin conditions like eczema or psoriasis.
If PN is caused by a mental health issue like depression or anxiety, consider counseling to address any underlying psychological factors.

Hidradenitis Suppurativa (HS)
Hidradenitis Suppurativa is another chronic skin condition that develops in areas where skin rubs together or where there are hair follicles. These areas include the armpits, groin, buttocks, and under the breasts in women.
HS begins with hard lumps or lesions under the skin. For some people, these lumps connect by tunnels under the skin, turning small areas into large sores. These areas can break open and turn into an abscess, causing significant pain and discomfort.
Causes and triggers of HS
The exact cause is unclear, but it’s often linked to obesity and Crohn’s disease.
Genetics may also lead to HS. Black people are more often affected by HS even after considering other factors like age, sex, body mass index, and tobacco use. Unfortunately, this leads Black people to utilize the healthcare system more often, trying to manage HS
Treatment options for HS
Treatment options for HS vary depending on how severe it is. Like other skin conditions, more than one treatment option may be needed. Some standard treatment options include10:
- Antibacterial washes or soaps, antibiotics or retinoids
- Oral Antibiotics
- Anti-inflammatory medications
- Biologic Therapies
- Oral contraceptives and other hormonal therapies
- Corticosteroids or other immunosuppressants
Along with medication options, managing HS may require lifestyle changes or invasive treatments. For example, weight loss and a healthy diet help improve symptoms, as obesity is linked to HS. Regular, gentle cleansing and applying a warm compress to inflamed areas can help.
More invasive options like laser or light therapies help target hard-to-treat areas. In more severe cases, surgical options may be considered. This can include draining abscesses, removing affected tissue, or, in extreme cases, removing whole sections of skin.
The Bottom Line
Skin conditions provide a unique twist that impacts our physical health and self-esteem. Most people know someone with eczema or psoriasis. Still, for other skin conditions, like prurigo nodularis or hidradenitis suppurativa, you may be surprised by what it takes to live with them daily.
Understanding Black people’s unique challenges with these conditions empowers us to advocate for more accessible, affordable solutions. Seeking specialized care from healthcare professionals or dermatologists who understand the nuances of Black skin conditions can significantly improve your quality of life.
Join us as we continue to advocate for and promote awareness of skin conditions that affect Black people.
Conversation Starters:
- Have you ever personally dealt with a skin condition, or do you know someone who has? How did it impact your/their daily life?
- Are there any skin conditions discussed in the article that you found particularly interesting or previously didn’t know about?
- Have you ever encountered misconceptions or stereotypes surrounding skin conditions? How do you think we can work to combat such stereotypes?
References
- Croce EA, Levy ML, Adamson AS, Matsui EC. Reframing racial and ethnic disparities in atopic dermatitis in Black and Latinx populations. J Allergy Clin Immunol. 2021;148(5):1104-1111. doi:10.1016/j.jaci.2021.09.015
- Lee JH, Son SW, Cho SH. A Comprehensive Review of the Treatment of Atopic Eczema. Allergy Asthma Immunol Res. 2016;8(3):181-190. doi:10.4168/aair.2016.8.3.181
- Alexis AF, Blackcloud P. Psoriasis in skin of color: epidemiology, genetics, clinical presentation, and treatment nuances. J Clin Aesthet Dermatol. 2014;7(11):16-24.
- Ludmann, Paula. “Vitiligo: Overview.” American Academy of Dermatology Association., 29 June 2022, www.aad.org/public/diseases/a-z/vitiligo-overview. Accessed 13 September 2023.
- NIAMS. “Vitiligo.” National Institute of Arthritis and Musculoskeletal and Skin Diseases, 12 Apr. 2017, www.niams.nih.gov/health-topics/vitiligo. Accessed 13 September 2023.
- “Vitiligo: MedlinePlus Genetics.” Medlineplus, 24 Feb. 2022, medlineplus.gov/genetics/condition/vitiligo/#causes. Accessed 13 September 2023.
- Kubelis-López, David Emmanuel et al. “Updates and new medical treatments for vitiligo (Review).” Experimental and therapeutic medicine vol. 22,2 (2021): 797. doi:10.3892/etm.2021.10229
- Prurigo Nodularis – Pruritic Rash – Skin Disease. rarediseases.org. Accessed September 18, 2023. https://rarediseases.org/rare-diseases/prurigo-nodularis/#affected
- Boozalis E, Tang O, Patel S, et al. Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol. 2018;79(4):714-719.e3. doi:10.1016/j.jaad.2018.04.047
- Mayo Clinic. Hidradenitis suppurativa – Symptoms and causes. Mayo Clinic. Published 2019. https://www.mayoclinic.org/diseases-conditions/hidradenitis-suppurativa/symptoms-causes/syc-20352306
- Byrd AS, Rosenberg AZ, Shipman WD, et al. Hidradenitis suppurativa in Black and White patients – a clinical study. Eur Rev Med Pharmacol Sci. 2023;27(3 Suppl):92-98. doi:10.26355/eurrev_202304_31325
- Ulschmid C, Serrano L, Wu R, Roth GM, Sokumbi O. African American race is a risk factor for severe hidradenitis suppurativa. Int J Dermatol. 2023;62(5):657-663. doi:10.1111/ijd.16428
You Might Also Like:

5 Skin Conditions Men Are More Susceptible To
In this article, we’ll break down five skin conditions men are more susceptible to, explain the science behind them, and share what can be done to prevent or manage them effectively.

Is Clinical Research for Your Skin Condition Right for You?
When it comes to our skin, we often focus on daily routines and readily available treatments. But have you ever considered if participating in clinical research could be a valuable step in your skin health journey? Learn more.









