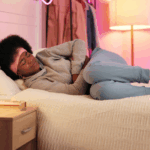
If you live with ulcerative colitis (UC), you know how unpredictable it can be. One day you’re fine, working, cooking, showing up, and the next, your body feels like it’s turned against you. A flare-up can make simple routines like eating breakfast or leaving the house feel impossible.
UC is a chronic inflammatory bowel disease that causes swelling and ulcers in the lining of your colon and rectum. It comes in waves — quiet periods of remission, followed by flares when inflammation returns.1
The condition affects people of all backgrounds, but Black and Brown communities often experience longer delays in diagnosis, less access to gastroenterologists, and higher rates of hospitalization.1
Still, living with UC doesn’t mean surrendering to it. With the right tools, care, and support, you can regain control and stay ahead of flares before they control you.
This is your practical, no-nonsense guide to beating a UC flare-up, without breaking the bank.
What a Flare-Up Looks Like
A UC flare-up happens when inflammation in your colon reignites.2 The protective lining of your gut becomes irritated and begins to bleed or ulcerate, triggering symptoms like:
- More frequent or urgent bowel movements.2
- Abdominal pain or cramping that worsens after meals.2
- Fatigue or low energy.2
- Mucus or blood in stool.2
- Nausea or loss of appetite.2
Some flares creep in slowly, while others hit fast. Triggers can include infections, stress, changes in medication, or certain foods.2
Early recognition is everything. When you know what’s happening, you can act fast and that can make all the difference.
1. Act Early: Track and Communicate
UC doesn’t wait and neither should you. The earlier you notice a flare starting, the easier it is to manage. Start by tracking your symptoms daily. You can jot notes in your phone or use free apps like Cara Care or MySymptoms.
Record bowel movements, energy levels, food intake, stress, and any medication changes. This log can help your doctor spot early inflammation or medication issues before they become severe.
If you notice symptoms lasting more than 48–72 hours, call your gastroenterologist or primary care provider.3 Ask specifically for:
- CRP (C-reactive protein): shows inflammation in the blood.3
- Fecal calprotectin test: detects inflammation in the colon.3
- Basic bloodwork: checks for anemia or dehydration.3
Cost-conscious tip: If specialty appointments are expensive, start with a telehealth visit or community clinic. Many labs, like Quest and Labcorp, now offer discounted patient-direct testing for inflammation markers that you can order yourself.
2. Eat for Calm, Not Chaos
When you’re flaring, your gut is sensitive and inflamed. The goal isn’t a trendy cleanse; it’s giving your intestines a break while staying nourished.
What to eat:
- Low-fiber, gentle foods: oatmeal, rice, eggs, potatoes, applesauce, bananas, white bread, plain pasta.4
- Soups and broths: easy to digest and restore lost electrolytes.4
- Lean proteins: chicken, turkey, tofu, or soft fish help with healing.4
- Small meals more often: instead of three big meals, try five small ones to reduce strain on the gut.4
- Fried, spicy, or high-fat foods that irritate the colon.4
- Caffeine, alcohol, and carbonated drinks.4
- Dairy (if you notice increased bloating or cramping).4
- Raw veggies, seeds, and high-fiber foods until symptoms improve.4
Budget-friendly swaps: You don’t need expensive “gut health” powders. Stick to frozen fruits and veggies, store-brand oatmeal, and homemade electrolyte drinks (1 liter of water + ½ tsp salt + 6 tsp sugar).
Once you’re stable, reintroduce fiber gradually. Think cooked carrots, peeled apples, or mashed sweet potatoes.4
3. Manage Stress (Because the Gut Feels Everything)
Your gut and brain are in constant conversation. When you’re under stress, your body releases cortisol and adrenaline, which are critical hormones that can worsen inflammation and disrupt digestion.5
Managing stress doesn’t require expensive retreats. It’s about building small, restorative moments into your day:
- Deep breathing: inhale for 4 seconds, hold for 4, exhale for 4 — repeat for 5 minutes.
- Gentle movement: yoga, stretching, or walking helps relieve cramping and improve circulation.
- Digital detox: silence notifications, limit doom-scrolling, and prioritize rest.
- Free resources:
- YouTube yoga and meditation channels like “Yoga With Nico” or “Arianna Elizabeth”.
- Insight Timer app for guided relaxation (free).
- Community counseling programs through churches or local nonprofits for low-cost therapy.
- YouTube yoga and meditation channels like “Yoga With Nico” or “Arianna Elizabeth”.
Stress is a flare’s silent fuel. Learning to manage it is one of the most powerful medicines you can give yourself.
4. Rebuild and Restore After a Flare
When a flare subsides, your body is depleted. Rebuilding your energy and nutrients helps prevent the next one.
Ask your provider to check your iron, vitamin D, B12, and folate, as deficiencies are common with UC and can worsen fatigue.6 If lab work is expensive, check community health centers or LabCorp’s low-cost wellness panels.
Affordable food-based recovery options:
- Iron: lentils, spinach, canned tuna, or fortified cereals.7
- Vitamin D: eggs, mushrooms, and 15 minutes of sunlight.7
- B12: yogurt, milk alternatives, or chicken.7
- Probiotics: instead of pricey capsules, try kefir, yogurt, or sauerkraut to restore gut bacteria.7
Hydration is key: Aim for 2–3 liters of fluid daily, especially if you’ve lost fluids during a flare. And most importantly, rest. Your gut can’t heal if you’re running on empty.
5. Stay Connected and Advocate for Your Health
UC can make you feel isolated, but connection changes everything. Sharing your experience, asking questions, and learning from others can reduce anxiety and help you make informed decisions.
Find your people:
- Join UC and IBD support groups, online or in person, that center Black and Brown voices.8
- Talk openly with family and friends so they understand your triggers and support your boundaries.8
- Follow credible advocacy organizations like the Crohn’s & Colitis Foundation and Color of Gastrointestinal Illnesses (COGI), which address racial disparities in IBD care.
Advocate at appointments:
- Bring your symptom log.
- Ask, “What’s our plan if this flare doesn’t improve?”
- Request access to a nutritionist or mental-health provider familiar with UC.
If cost is a barrier:
- Ask about patient-assistance programs from medication manufacturers.
- Some nonprofits cover co-pays for infusions or offer free transportation for appointments.
Advocacy isn’t confrontation, it’s self-protection. Your story deserves to be heard.
Understanding the Disparity
Research shows that Black and Hispanic UC people are less likely to be referred to a gastroenterologist, less likely to receive advanced treatments, and more likely to experience complications or hospitalization.1
Many also face longer wait times for diagnosis, sometimes years, due to misattributed symptoms, healthcare bias, and financial barriers.1 These disparities highlight why education and community are essential parts of treatment.
Knowing your body, tracking your symptoms, and demanding timely care isn’t just good medicine, it’s health equity in action.
References
- Florence-Damilola, O., Aboubakr, A., & Anyane-Yeboa, A. (2022). INFLAMMATORY BOWEL DISEASE IN UNDERSERVED POPULATIONS: LESSONS FOR PRACTICE. Current Opinion in Gastroenterology. doi:10.1097/MOG.0000000000000855
- Klein, E. (2024, March 28). What to Know (and Do) About Ulcerative Colitis Flare-Ups. Retrieved from Healthline: https://www.healthline.com/health/ulcerative-colitis-take-control-dealing-with-flares
- AGA . (2023, February 21). New AGA guideline recommends blood and stool tests for monitoring ulcerative colitis. Retrieved from The American Gastroenterological Association (AGA): https://gastro.org/press-releases/new-aga-guideline-recommends-blood-and-stool-tests-for-monitoring-ulcerative-colitis/
- The Crohn’s & Colitis Foundation. (2025). What Should I Eat with IBD? Retrieved from The Crohn’s & Colitis Foundation: https://www.crohnscolitisfoundation.org/patientsandcaregivers/diet-and-nutrition/what-should-i-eat
- Osso, M., & Riehl, M. (2024, August 7). Stress and IBD: Breaking the Vicious Cycle. Retrieved from The Crohn’s & Colitis Foundation: https://www.crohnscolitisfoundation.org/blog/stress-and-ibd-breaking-the-vicious-cycle
- Issokson, K. (2017). Common Micronutrient. Retrieved from The Crohn’s & Colitis Foundation : https://www.crohnscolitisfoundation.org/sites/default/files/legacy/science-and-professionals/nutrition-resource-/micronutrient-deficiency-fact.pdf
- Espinosa-Salas, S., & Gonzalez-Arias, M. (2023, September 21). Nutrition: Micronutrient Intake, Imbalances, and Interventions. Retrieved from StatPearls: https://www.ncbi.nlm.nih.gov/books/NBK597352/
- The Crohn’s & Colitis Foundation. (2025). Community and Support. Retrieved from The Crohn’s & Colitis Foundation : https://www.crohnscolitisfoundation.org/patientsandcaregivers/community-support?trackBlock=true&blockTitle=patient-and-caregiver-education-programs&referencedPageTitle=myibd-learning-events